Introduction
There are over 350 million people in the world living with arthritis. This widespread condition has a huge effect on day-to-day activities, from hobbies and interests to essential skills like dressing and cooking. It’s painful, ever-changing, and causes our joints to become swollen and stiff. With there being so many different types of arthritis, no two cases are the same and every person experiences it differently.
The good news is, there’s lots you can do to help symptoms of all types of arthritis. A great example is compression therapy, which is one of our biggest passions here at Grace & Able. Read on to find out more about what types of arthritis are out there and how compression therapy can help them.
What is Arthritis?
When we use the word ‘arthritis’, it’s more of an umbrella term than a specific condition. In simple terms, it’s a collection of joint disorders that cause inflammation in one or more joints. This includes knuckles, knees, wrists, and ankles.
Most people think of arthritis as something that only affects the elderly, but this isn’t necessarily true. Whilst age is often a contributing factor, and arthritis is generally more common in older people, arthritis can affect people from early childhood. With it being a chronic condition, arthritis doesn’t have a cure and often gets worse over time. However, it can be managed with a multifaceted approach involving medications, exercise, surgery, and a wide range of therapies.
Types of Arthritis
Now we know what arthritis is, it’s time to look at just some of the 100+ types of arthritis. Whilst there’s plenty of crossover between the types and their symptoms, each one affects the body slightly differently and has its own combination of symptoms and causes. It’s important to get a doctor’s diagnosis when it comes to types of arthritis, as your treatment plan and prognosis will depend on which specific type you have.
1. Osteoarthritis (OA)
The most common type of arthritis is Osteoarthritis or OA. It usually develops in people in their mid-40s or older, but can come on at any age as a result of an injury or another joint-related condition like gout or rheumatoid arthritis. Generally, osteoarthritis affects more women than men and is more common in people who have family with the condition.
Osteoarthritis starts by affecting the smooth cartilage lining that cushions the joint, wearing it down over time and causing pain and stiffness. As this lining gets thinner and rougher, the tendons and ligaments have to work a little harder to support the joint, causing swelling and the formation of bone spurs, known as osteophytes. Over time, the loss of cartilage makes your bones rub against each other, changing the shape of the joint and forcing the bones to move out of their normal position.
Symptoms:
-
- Joint pain and stiffness
- Swelling around the affected joint
- Tenderness
- Reduced range of motion
- Clicking, grating, or crackling sounds when moving the affected joints
Causes & Risk Factors:
-
- Aging - osteoarthritis is more common in older people
- Joint injury especially if a joint has not healed after an injury or operation
- Obesity - excess weight means excess strain on joints, especially your knees and hips
- Family history - it’s thought that osteoarthritis may run in families, but studies are yet to identify a single gene responsible
- Other conditions (secondary arthritis) - if you have a condition that damages your joints, such as gout, this can cause osteoarthritis
2. Rheumatoid Arthritis (RA)
Rheumatoid arthritis is an autoimmune disease where your immune system mistakenly attacks the lining of your joints, making them stiff, sore, and swollen. As the disease progresses, it starts to damage your joints, cartilage, and bones, causing the joint to lose its shape and become out of place. Nobody knows exactly why rheumatoid arthritis happens, but theories like an infection triggering the immune system or a genetic source have been studied.
Symptoms:
-
- Persistent throbbing and aching pain in the joints
- Stiff joints that make movement difficult
- Swelling, warmth, and redness that makes the joints hot and tender to touch
- Additional symptoms like fatigue, fever, sweating, weight loss, and a poor appetite
Causes & Risk Factors:
-
- Genetics - there’s evidence to suggest that RA can run in families, but the risk is thought to be low
- Autoimmune triggers - whilst not proven, it’s been theorized that previous illness and infections can cause autoimmune conditions
- Smoking - it has been suggested that people who smoke have a higher risk of developing the condition
- Hormonal changes - there may be a link between the female hormone oestrogen, but this hasn’t been proven
3. Psoriatic Arthritis (PsA)
This type of arthritis affects some people with psoriasis, a skin condition that causes flaky patches of skin that form silvery scales. Not everyone who has psoriasis will get psoriatic arthritis, but those who do tend to develop it as they get older, many years after a psoriasis diagnosis. It’s not clear why some people with psoriasis get it whilst others do not.
Symptoms:
-
- Sore, stiff, swollen joints
- Swollen fingers and toes
- Nail changes including pitting, colour changing, crumbling, and separation from nail beds
- Pain in your feet, especially at the back of your heel or the sole of your foot
- Fatigue and lack of energy
Causes & Risk Factors:
-
- Family history - having family members with psoriasis and/or psoriatic arthritis increases the likelihood of you having it
- Immune system dysfunction - psoriasis and psoriatic arthritis are autoimmune disorders where your immune system attacks healthy cells
4. Gout
Gout happens when there’s too much uric acid in your blood. Too much uric acid leads to little crystals forming around your joints, causing pain and inflammation. When we think of gout, we usually think of rich medieval monarchs or millionaires living unhealthy lifestyles, but gout can affect anyone. It comes in waves, known as attacks or flare ups, which can come back anywhere between every few months or every few years.
Symptoms:
-
- Sudden, intense joint pain (often in your big toe, but it can be in any other joints)
- Swollen, hot, red skin over the joint
- Swelling and tenderness
- Fatigue and generally feeling unwell
- Fever and chills
Causes & Risk Factors:
-
- High purine diet - eating lots of red meat, organ meats, and certain seafood
- Binge drinking - excessive alcohol use increases the amount of uric acid in your blood
- Obesity - being overweight increases the risk of gout
- Kidney disease - kidney problems prevent the body from getting rid of excess uric acid
- Certain medications - things like diuretics and ACE inhibitors can lead to a higher risk of gout
- Other conditions like high cholesterol, high blood pressure, osteoarthritis, diabetes, or surgeries and injuries
5. Ankylosing Spondylitis
Sometimes known as AS, ankylosing spondylitis is a type of axial spondyloarthritis that causes inflammation in the spine and other areas of the body. It tends to first develop in teenagers and young adults. It’s a chronic condition that will affect people for life and there’s no cure or way to reverse damage done. Some people with AS are able to live independently with minimal disability, whilst others can become severely disabled and end up with a fused spine which makes mobility exceptionally difficult.
Symptoms:
-
- Back pain and stiffness
- Pain, swelling, and warmth in the joints
- Fatigue and lack of energy
- Enthesitis (inflammation where the bone is joined to a tendon or ligament)
- Other conditions like iritis, psoriasis, and inflammatory bowel disease
Causes & Risk Factors:
-
- Genetics - 8 out of 10 people with AS carry a gene variant known as HLA-B27
The Role of Compression Gloves in Arthritis Management
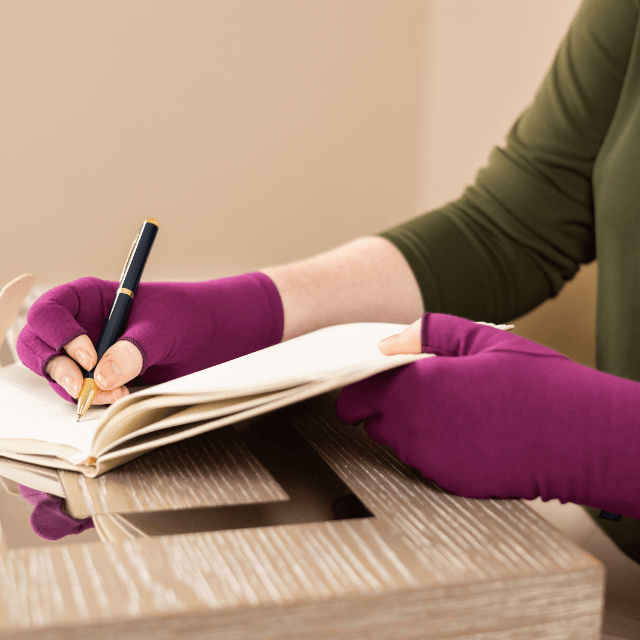
Arthritis often affects the joints in your hands and fingers. This can be particularly difficult because we use our hands almost constantly, and they’re a vital part of our everyday activities. If your hands are painful, stiff, and swollen, these everyday activities become much harder. Using compression gloves helps lessen these symptoms whilst supporting your joints to move better.
Benefits of Compression Gloves:
1. Pain Relief
Compression gloves apply pressure to the joints, improving blood circulation and reducing inflammation, which in turn, helps ease and prevent pain.
2. Improved Mobility
Because compression gloves help to support the joints and reduce stiffness, they make it easier to move your hands without causing more pain. This makes it easier to do your normal activities and remain independent.
3. Reduced Swelling
The gentle compression pushes out fluid, preventing fluid buildup. This helps reduce the swelling in your hands.
4. Enhanced Warmth
Ever notice your arthritis symptoms getting worse in cold weather? Like normal gloves, compression gloves keep your hands nice and warm whilst applying a bit of heat therapy to soothe stiff and achy joints.
5. Support for Nighttime Relief
Morning stiffness is very common in people living with arthritis. Wearing your compression gloves overnight prevents this stiffness, allowing for a more comfortable start to the day.
How to Choose the Right Compression Gloves
Looking for your first pair of compression gloves? You’re in the right place! It can feel like a bit of a minefield picking your first pair because there’s so many different types. Here’s a few things to consider:
1. Material
Since you’ll be wearing your compression gloves quite a lot, you’re going to want something as comfy as possible. Breathable, stretchy fabrics with moisture-wicking properties like cotton blends are perfect for this.
2. Fit and Compression Level
To get the most out of your compression gloves, you need them to give a gentle compression. A nice, snug fit is really important, but make sure they’re not so tight they restrict circulation!
3. Fingerless vs. Full-Finger Gloves
-
- Fingerless gloves: These offer greater dexterity and allow you to use touchscreen devices like your phone or tablet.
- Full-finger gloves: These are better for people with severe symptoms or people who live in cold climates and need full warmth and coverage.
Tips for Using Compression Gloves Effectively
-
- Consistency is key: For best results, make sure you’re wearing your compression gloves regularly, if not daily, especially if you’re doing activities that put strain on your joints.
- Combine with other treatments: Compression gloves are great, but they’re not the only treatment for arthritis and shouldn’t be used as such. Make sure you’re following your doctor’s instructions when it comes to medication and physiotherapy regimes, as well as any alternative treatments.
- Keep them clean: We know this sounds obvious, but don’t underestimate the power of a good clean! Keeping your compression gloves clean is important in making sure they work properly and last for a long time.
- Monitor for comfort: Our bodies change all the time, especially if you’re living with arthritis. If your gloves start to feel too tight or uncomfortable, it might be time to try a different size,
- Other Options for Arthritis Relief
Aside from medication and surgery (which are both really important!), there’s plenty more therapies that can provide arthritis relief. Remember to consult your physician before trying anything new and do your research.
1. Regular Exercise
Exercise can be difficult if you’re living with arthritis, but it’s important to keep your body moving as much as you can to keep inflammation down. Low-impact exercise is best because it prevents injury, which can make symptoms worse. Things like swimming, walking, yoga, and small stretches on your affected joints are all excellent for reducing symptoms.
2. Anti-Inflammatory Diet
A balanced diet is crucial to keeping symptoms at bay and keeping yourself fit and healthy. Some people may find an anti-inflammatory diet rich in omega-3 fatty acids, fruits, vegetables, and whole grains beneficial in reducing inflammation.
3. Hot and Cold Therapy
Just like you’d put a hot water bottle on a sore belly or an ice pack on a bruised knee, hot and cold therapy can be great at soothing sore joints, reducing stiffness, and preventing swelling.
Frequently Asked Questions
Q: What’s the most common type of arthritis?
A: The most common type of arthritis is osteoarthritis. According to the CDC, it affects over, 32.5 million adults in the US.
Q: How is arthritis diagnosed?
A: Diagnosing arthritis can be tricky, especially when it comes to working out which type you have. Your doctor will usually take your medical history and perform a physical exam before ordering blood tests, X-rays, MRI scans, and/or joint fluid analysis. The way you’re diagnosed will depend on your symptoms and presentation, so this will be different for everyone.
Q: Can I wear compression gloves to bed?
A: Absolutely! Grace & Able compression gloves are designed with skin-kind labels for sensitive skin and made using super-soft materials, so they’re perfect for wearing day and night. You may want to size up for overnight wear as hands can swell in your sleep, but this is up to you.
Q: How do I clean my compression gloves?
A: We recommend hand washing Grace & Able Compression Gloves in cool water and air drying. If it is difficult for you to hand wash, another option is to put them in a machine wash on a low heat. Do not put in the dryer as hot washes and drying can shrink the fabric.
Ready to start your compression therapy journey? Our compression gloves are designed to be comfy whilst still looking pretty and complementing your style! Find your fit today and get ready to enjoy a supported, soothed experience.











































































Share and get 15% off!
Simply share this product on one of the following social networks and you will unlock 15% off!